Though we don’t talk about it much as a society, most Americans say that when the time comes, they want to die peacefully in their own homes. Unfortunately, many of us will not get that chance. Many deaths in this country continue to take place in hospitals or nursing homes, often due to complications of overtreatment.
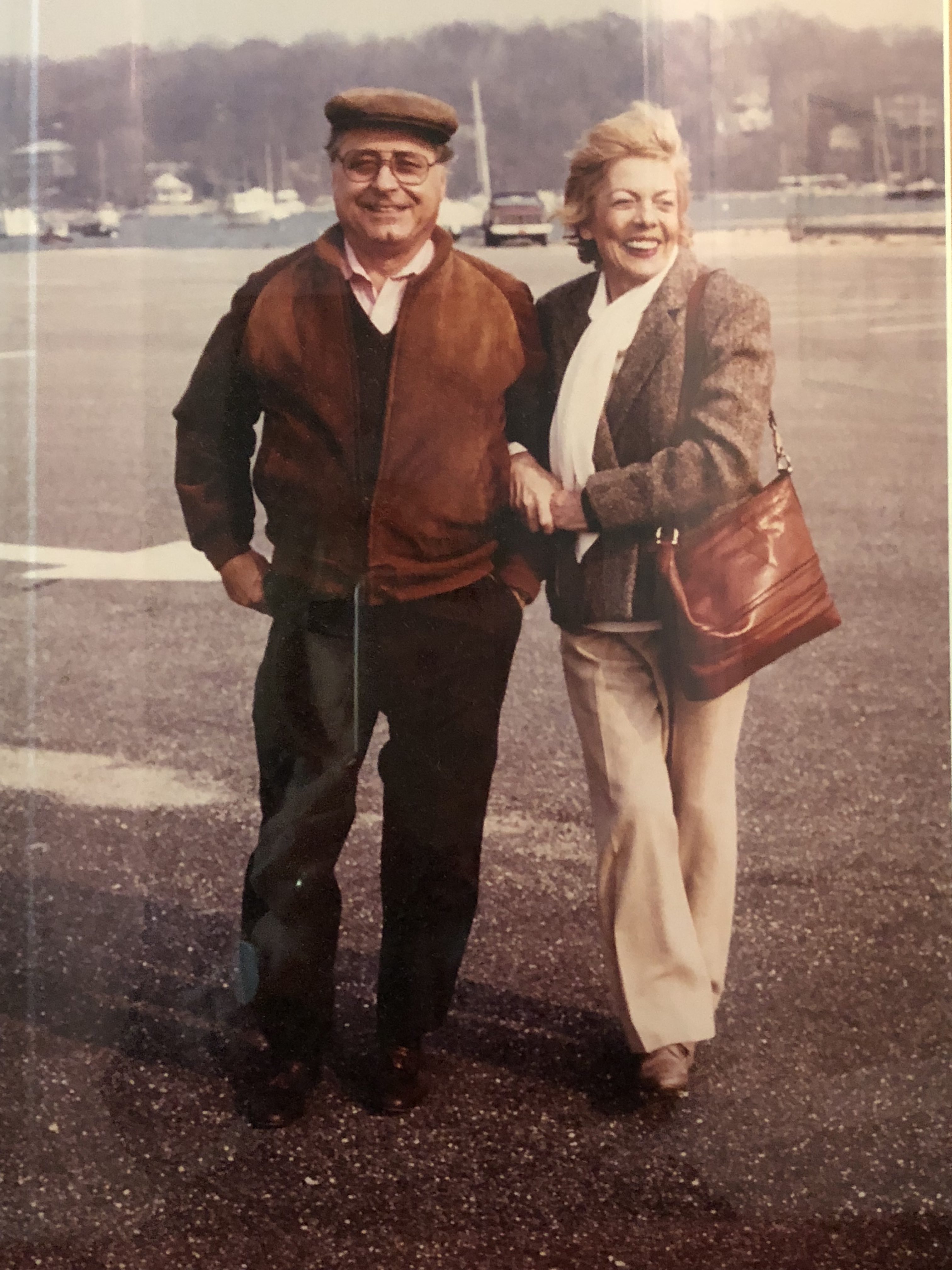
My dad, Robert Hochman, and my mom, Ara Montagnoli Hochman
My dad died that way at a hospital on the East Coast years ago after suffering a massive stroke. When I reflect on the experience, I remember what a chaotic and agonizing time it was for him and our family. I often wonder how things might have been different if we had a more realistic conversation with the clinicians about his prognosis. Would his passing have been more peaceful if he had a care plan that focused on quality of life and comfort as opposed to continued aggressive treatments?
My mother’s death, on the other hand, was the complete opposite experience. After battling metastatic colon cancer, she lived her final days at home. She passed away peacefully in bed, surrounded by loved ones, exactly the way she wanted. It was a sacred time for our family that I will treasure forever.
All of us have a story about the loss of a loved one. It’s something that affects everyone eventually. The sad reality, however, is that care for incurably ill people remains one of the most broken parts of the U.S. health system. But this is about more than just end-of-life care. I have said many times, if we can improve the patient experience in the last two years of life, we will go a long way toward improving health care for people at every stage of life.
That’s why Providence St. Joseph Health is deeply committed to delivering better care through the end of life. It starts with clinicians talking to patients early on about what kind of care they would want in the event they become incapacitated. It’s about listening intently to our patients to understand what matters most to them so we can help them live the best life possible in whatever time they have ahead.
Through our Institute for Human Caring, led by Ira Byock, M.D., we are creating a culture in which these conversations are a part of routine care. We call this approach whole person care. When you’re a patient with us, we want to know what you care about most, so we can partner with you to achieve it. Here are five ways we’re making this the new normal at Providence St. Joseph Health:
- We engage patients in shared decision-making to clarify achievable outcomes and the person's goals for care prior to potentially burdensome treatments.
- We encourage every adult patient to have an advance directive on file, naming someone they trust to speak for them in the event they’re unable to speak for themselves due to an incapacitating medical condition.
- We’ve optimized our electronic health record system to give providers a full view of a patient’s goals for care and advance directives. This is a great example of how we’re shifting every aspect of our culture – including our IT philosophy – to a whole person care paradigm.
- We prescribe simple, fact-based videos and other resources to help patients understand their medical conditions and options for care near the end of life through our partnership with ACP Decisions.
- We provide tools and training for our caregivers to help them address the holistic needs of our patients in every health care setting through our collaboration with the Center to Advance Palliative Care.
At some point, we must all take the inevitable step of dying. Walking alongside patients during this final chapter is one of the greatest privileges we are given as clinicians. Just as we strive to help people live well throughout their lives, we owe it to them to support them in dying well. We still have a long way to go as a nation, but understanding what matters most to patients is a fundamental first step.
Have you completed an advance directive?
It’s never too early to plan for the care you want in the event you are unable to speak yourself. The Institute for Human Caring at Providence St. Joseph Health has developed helpful resources to help you plan ahead. CHECK OUT OUR STEP-BY-STEP GUIDE>>
Stories that inspire us
Patients, families and caregivers can teach us so much about what it means to live fully, especially as they near the end of life. We’ve captured some inspiring stories as part of our Hear Me Now series, a partnership with StoryCorps. LISTEN>>


